22-Year-Old Fatally Shot During Random Home Invasion By Career Criminal

A North Carolina college student was shot and killed while visiting friends in Columbia, South Carolina, during a violent home invasion by a repeat offender with a long criminal record. Authorities have arrested 30-year-old Alexander Dickey, who now faces multiple felony charges in connection with the incident.
LISTEN TO THIS ARTICLE
COLUMBIA, SC (4-minute read) — A tragic crime has shaken the Columbia, South Carolina, community after a 22-year-old college student from North Carolina was fatally shot during a random home invasion on May 3.
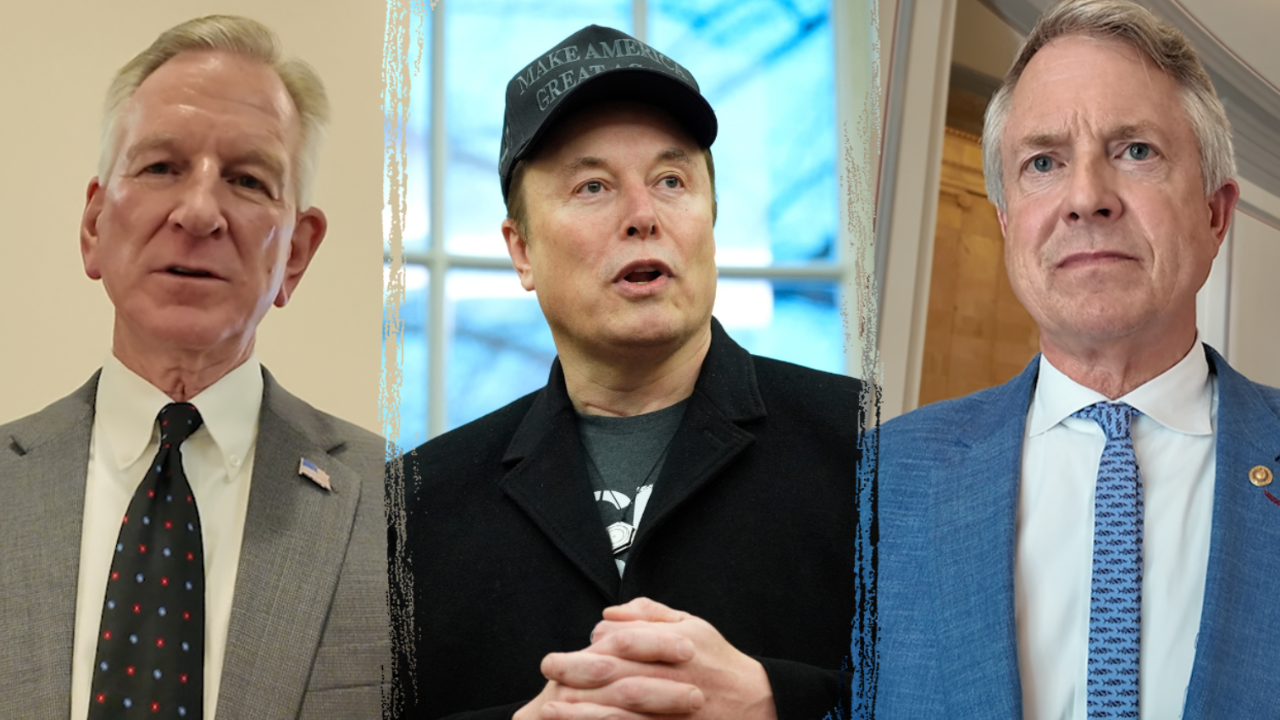
Logan Federico, a devoted aspiring teacher from Waxhaw, NC, was visiting friends and staying overnight at a residence on Cypress Street. According to Columbia Police Chief Skip Holbrook, the intruder, identified as 30-year-old Alexander Dickey, broke into the home and shot Federico in the chest after stealing credit cards. The case, described by police as a random act of violence, underscores the danger posed by repeat offenders.
Dickey is a career criminal with a staggering record — 40 criminal and traffic offenses since 2013. His history includes burglary, larceny, robbery, resisting arrest, and possession of stolen property. On the morning of the incident, he allegedly drove a stolen vehicle into the neighborhood, burglarized a nearby home to steal another vehicle and a firearm, and then broke into the house where Federico was staying.
After the fatal shooting, Dickey fled, using the stolen credit cards on a shopping spree. When his stolen vehicle broke down, he called a tow truck to transport it to a home in Gaston. Law enforcement tracked him to that location on May 3, prompting a manhunt after he fled on foot. The next day, a local resident spotted him emerging from the woods and stealing another car. He returned to the Gaston house and forced his way inside, but police quickly surrounded the home and arrested him.
Dickey now faces a litany of charges, including murder, first-degree burglary, multiple counts of theft, and illegal possession of a firearm as a convicted felon.
Why Securing Firearms Is Critical for Home and Guest Safety
One of the most alarming elements of this tragic case is that the suspect reportedly accessed a firearm during the first break-in—one that had not been properly secured. This raises a crucial point for all firearm owners: the importance of responsible firearm storage.
Whether you’re a gun owner yourself or staying in a home where firearms are present, unsecured firearms can quickly turn a burglary into a fatal incident.
Firearms in a home are intended to be tools for protection, but when improperly stored, they can be stolen and used for violence. In the context of home invasions, a securely stored firearm may prevent a criminal from gaining a deadly advantage.
For those who carry concealed, remember: even when you’re at home, firearm responsibility doesn’t end when the holster comes off. Quick-access safes allow you to store your firearm responsibly while still being able to access it in an emergency.
Firearm owners must treat storage with the same seriousness as they do training, maintenance, and carrying.
A Father’s Grief and a Community in Mourning
During a press conference, Logan’s father, Stephen Federico, tearfully honored his daughter, describing her as passionate, loving, and dedicated to working with children. “You can’t kill my spirit,” he said, echoing what he believed his daughter would have said to her attacker.
This tragic incident brings renewed focus on the issue of career criminals repeatedly returning to the streets, often with fatal consequences. It also highlights the importance of vigilance, situational awareness, and community cooperation in preventing and responding to such threats.
Safety Tip: Always secure doors and windows, even during the day. If you’re visiting or staying in an unfamiliar home, ensure everyone is aware of emergency procedures and knows where firearms or self-defense tools are stored, and confirm they are safely secured but accessible to those trained to use them.
Read the full article here